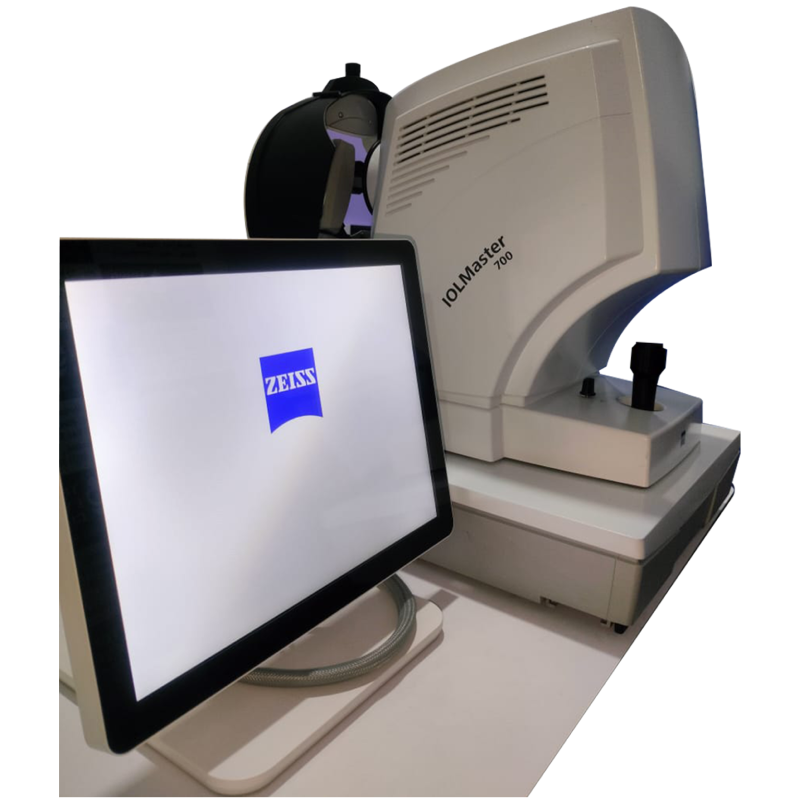
Use of IOL Master (IOLMaster 700)
The IOLMaster 700 by ZEISS is an advanced ocular biometer widely used in ophthalmology, especially for patients undergoing cataract surgery. Its primary purpose is to provide highly accurate biometric measurements of the eye, which are essential for calculating the correct intraocular lens (IOL) power. This ensures that after surgery, patients achieve the best possible visual outcome with minimal dependence on glasses.
One of its key functions is the measurement of axial length, which is the distance from the cornea to the retina. This measurement plays a critical role in determining the IOL power. The device also performs keratometry, which assesses the curvature of the cornea, helping in the detection of astigmatism and aiding in the planning of toric IOLs. Additionally, it measures anterior chamber depth, lens thickness, and white-to-white distance, all of which are important for precise surgical planning.
The IOLMaster 700 also supports toric IOL planning, allowing surgeons to choose and align toric lenses for patients with astigmatism. Since the device is non-contact and quick, it is comfortable for patients and efficient for clinical workflow. Its advanced formulas and precise imaging technology provide superior accuracy compared to older biometry methods, making it the gold standard in modern cataract surgery preparation.
Use of Visual Field Analyzer (VFA)
The Visual Field Analyzer (VFA) is one of the most important tools in modern eye care because it provides a complete picture of how well a patient can see in both central and peripheral areas of vision. Unlike standard eye charts, which only test how clearly someone can see letters or symbols straight ahead, the VFA examines the entire scope of vision. This makes it especially valuable for detecting conditions that may not affect central vision at first but cause subtle side vision loss, such as glaucoma. Identifying these changes early allows doctors to start treatment before permanent vision damage occurs.
Beyond glaucoma, the VFA is widely used in cases of optic nerve diseases (like optic neuritis or ischemic optic neuropathy) and retinal problems that can affect how light is detected. It also has great importance in neurology, since certain brain conditions—such as stroke, brain tumors, or pituitary gland disorders—can lead to characteristic visual field defects. By analyzing the pattern of vision loss, doctors can often determine where along the visual pathway a problem exists.
The test itself is non-invasive and simple for patients. They are asked to look at a central point inside the machine while small lights are presented in different parts of the screen. The patient presses a button each time they see a light, and the analyzer records their responses to create a detailed map of vision sensitivity. Advanced software also allows doctors to compare results over time, which is vital for tracking disease progression and adjusting treatments accordingly.

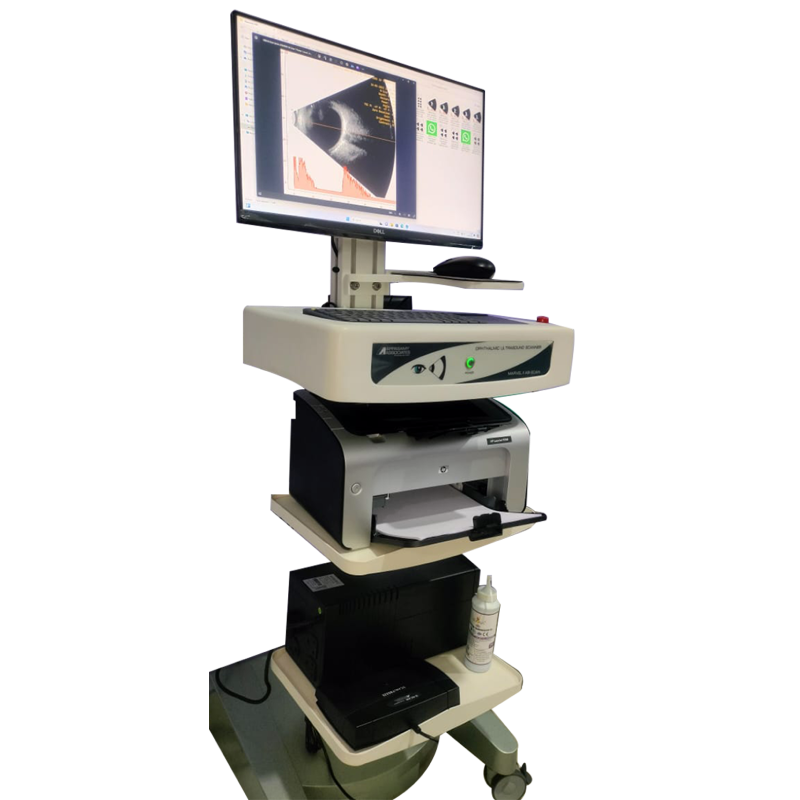
Use of B-Scan Ultrasonography (Ophthalmic B-Scan)
The B-Scan is a diagnostic test that uses high-frequency sound waves to create a cross-sectional image of the eye and the orbit. It is especially valuable when direct visualization of the retina or other internal eye structures is not possible due to media opacities like dense cataract, corneal opacity, or vitreous hemorrhage.
One of its primary uses is in the detection and evaluation of retinal detachment, vitreous hemorrhage, intraocular tumors, and foreign bodies. It can also help in diagnosing posterior vitreous detachment, choroidal detachment, intraocular inflammation, and trauma-related complications. By providing detailed information about the posterior segment, the B-scan often guides the ophthalmologist in making surgical or treatment decisions when a standard fundus examination is not possible.
The test is non-invasive and safe. A probe is placed gently on the closed eyelid (or sometimes directly on the eye with anesthetic drops), and ultrasound waves are used to create a two-dimensional image on the monitor. The resulting scan gives the doctor a clear picture of the structures behind the lens and cornea, which cannot be seen with normal examination tools in cases of opacity.
Use of OCT (Optical Coherence Tomography)
Optical Coherence Tomography (OCT), as seen in the Zeiss CIRRUS HD-OCT system in the image, is a revolutionary imaging technology that has significantly enhanced the way eye diseases are diagnosed and monitored. It provides high-resolution, cross-sectional, and three-dimensional images of the retina and other ocular structures using light waves, similar to how ultrasound uses sound waves. One of its most valuable features is the ability to detect minute changes in retinal structure that are invisible during a standard clinical examination, allowing for earlier intervention and better outcomes in diseases that can lead to vision loss.
In retinal care, OCT is indispensable for diagnosing and tracking conditions like age-related macular degeneration (AMD), where it helps detect drusen or fluid under the retina; diabetic retinopathy, by revealing macular swelling or bleeding; and macular holes or puckers, which can affect central vision. In glaucoma management, OCT aids in measuring the retinal nerve fiber layer and optic nerve cupping, helping detect early structural damage even before visual field loss becomes apparent. Furthermore, it assists in evaluating the vitreoretinal interface, identifying conditions like vitreomacular traction or epiretinal membranes. OCT is also valuable in preoperative assessment and postoperative monitoring, particularly after cataract or retinal surgeries, to ensure that healing is progressing normally and to detect any complications.
The procedure is quick, non-contact, and completely painless, making it suitable for regular use in clinical settings. Patients simply rest their chin on a support and focus on a target light while the device captures images in seconds. Its repeatability and precision make it ideal for tracking disease progression over time. As a result, OCT has become an essential part of standard ophthalmic practice, guiding clinical decisions, tailoring treatments, and improving patient outcomes through early and accurate diagnosis.

Use of Yag laser
The machine shown in the image is a YAG laser system, specifically the APPA YAG Laser, commonly used in ophthalmology for therapeutic laser procedures. YAG stands for Yttrium-Aluminum-Garnet, which is the crystal medium used to produce laser light at a wavelength of 1064 nm. This laser is primarily utilized for two important eye procedures: posterior capsulotomy and peripheral iridotomy. Posterior capsulotomy is often performed after cataract surgery when a patient develops posterior capsule opacification (PCO), a condition where the membrane behind the artificial intraocular lens becomes cloudy and affects vision. The YAG laser creates a small opening in this membrane to restore clear vision, usually with immediate effect. Peripheral iridotomy, on the other hand, is used to treat or prevent angle-closure glaucoma by creating a small hole in the iris to allow fluid to circulate more freely within the eye, thereby reducing intraocular pressure.
The procedure is non-invasive, painless, and done in a clinical setting. Patients are seated comfortably at the laser unit, similar to an eye examination at the slit lamp. Anesthetic drops are applied, and sometimes a special contact lens is used to stabilize the eye and focus the laser. The precision and safety of the YAG laser make it an essential tool in modern ophthalmic practice. In some cases, it may also be used for less common treatments such as managing vitreous floaters or performing gonioplasty. Overall, the YAG laser is a highly effective and efficient technology that significantly improves visual outcomes and quality of life for patients undergoing post-cataract or glaucoma-related treatments.

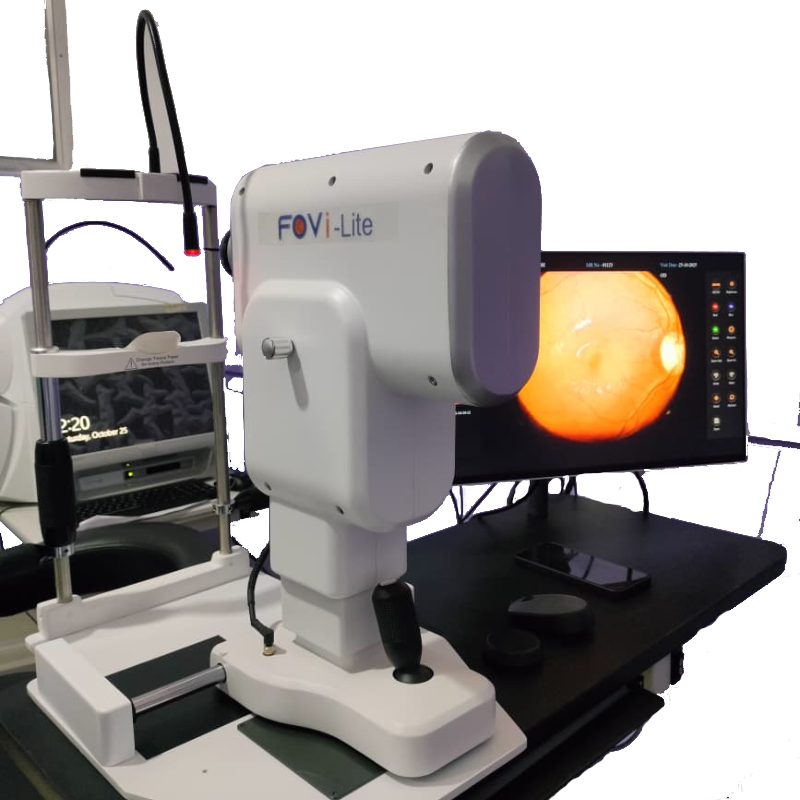
Use of Fovi Lite
At Third Eye Clinic, we use the advanced FOVi Lite non-mydriatic fundus camera to capture high-resolution images of the retina, macula and optic nerve for early detection and monitoring of eye conditions such as diabetic retinopathy, hypertension-related changes, glaucoma and age-related macular degeneration. This state-of-the-art device provides quick, comfortable and minimally invasive retinal imaging—often without the need for full pupil dilation—allowing our specialists to diagnose problems accurately and track disease progression over time. With digital documentation, precise imaging and expert evaluation, FOVi Lite helps us deliver safer, faster and more reliable retinal care to protect and preserve your vision.
we believe prevention is better than cure. By combining cutting-edge imaging (FOVi Lite) with skilled clinical expertise, we can help you preserve your vision for years to come.
📞 Call us today or book online to schedule your retinal imaging and full-eye check-up.
Use of Slit Lamp
At Third Eye Clinic, the slit lamp is one of our most essential diagnostic instruments, allowing our specialists to perform a detailed, magnified examination of both the front and back parts of your eye with exceptional clarity. Using a bright, focused beam of light combined with a powerful microscope, the slit lamp helps us assess the cornea, conjunctiva, sclera, iris, lens, vitreous, retina and optic nerve in high detail, enabling early detection of conditions such as cataracts, corneal ulcers, dry eye disease, uveitis, glaucoma, allergic reactions, infections and retinal abnormalities. This advanced evaluation method allows us to observe even the smallest structural changes, measure inflammation, check for foreign bodies, assess lens clarity, detect pressure-related damage and monitor chronic diseases over time. The procedure is completely safe, non-invasive and comfortable, taking only a few minutes while providing invaluable insights into your eye health. By combining slit-lamp imaging with our clinical expertise, Third Eye Clinic ensures precise diagnosis, personalized treatment planning and the highest standard of comprehensive eye care for every patient.